How AI Applications are changing Healthcare
Last Updated on October 19, 2024 by Editorial Team
Author(s): Igor Novikov
Originally published on Towards AI.

There have been a lot of changes recently in AI and the situation is evolving every day. It started proliferating in every industry, including healthcare and well-being.
Now, healthcare is a special beast because of the regulation and potential effects on human lives. Therefore adoption here is not as fast as some would have wanted, and different regulators like the FDA oftentimes drag their feet on approving new approaches.
So right now in healthcare AI mostly helps augment people in different routine tasks and rarely goes far in diagnosing and any sort of decision-making.
There are some notable attempts to change that, for example, Hyppocartic.ai tries to solve the nurse shortage problem and get an FDA approval.
The U.S. The Food and Drug Administration plays a crucial role in approving new treatment methods, including those that involve artificial intelligence and machine learning. The FDA’s role is to ensure that medical devices, treatments, and therapeutic methods are safe and effective for their intended use. For AI-based treatment methods, the FDA’s process generally follows similar principles to those used for traditional medical devices, with added emphasis on the unique challenges and characteristics of AI technology.
Here’s what the FDA requires for approval:
- Device Classification:
The FDA categorizes medical devices into three classes (I, II, and III) based on the level of risk they pose to patients.
- Class I: Low-risk devices, often subject to the least regulatory control (e.g., bandages).
- Class II: Moderate-risk devices, usually subject to more regulations (e.g., diagnostic tools, some AI-based systems).
- Class III: High-risk devices, requiring the highest level of scrutiny, often including clinical trials (e.g., AI-based devices used in critical care or surgical interventions).
AI-based medical technologies are typically classified as Class II or III, depending on the risk involved. If the AI solution plays a role in Clinical Decision Support or patient care and does not rely entirely on human decision-making, it may be classified as a medical device. This designation impacts the application’s compliance requirements, safety standards, and the pace at which updates or improvements can be made.
2. Premarket Submission Pathways:
- 510(k) Submission (Premarket Notification): For most Class II devices, this is the most common regulatory pathway. The manufacturer must demonstrate that the new device is substantially equivalent to an already legally marketed device (predicate device). For AI, substantial equivalence must be shown in terms of safety and efficacy.
- De Novo Classification: If no predicate device exists for a moderate-risk product, a De Novo submission can be filed to classify the new device, which includes AI-based technologies. This is for devices that are novel but present moderate risk.
- Premarket Approval (PMA): For Class III devices (high-risk), the PMA process requires significant clinical evidence to demonstrate safety and efficacy. This process is rigorous, and AI technologies used in critical applications (like diagnosis or life-saving interventions) may fall under this category.
3. Clinical Studies and Trials:
For AI-based treatment methods that present higher risks, the FDA often requires clinical trials to validate the technology’s safety and effectiveness. Clinical studies should include:
- Robust data on how the AI/ML model performs under various conditions.
- Analysis of the model’s accuracy, sensitivity, and specificity compared to existing treatments or tools.
- Testing the model’s generalizability to different populations and environments.
4. Good Machine Learning Practices (GMLP):
AI/ML-based technologies must follow the principles of GMLP, which include data quality, transparency, and validation. The FDA has begun outlining specific guidelines to ensure that AI models are developed and tested with the right datasets, reduce bias, and maintain patient safety.
5. Post-Market Surveillance:
The FDA monitors AI devices even after approval. AI systems that continue to learn or adapt after deployment (adaptive AI) might need continuous review to ensure that updates do not compromise safety or efficacy. This is part of the FDA’s evolving framework for “Software as a Medical Device” (SaMD).
For most startups trying to build healthcare systems, this process is very expensive and usually way too long. And AI systems add their own set of problems, especially around three areas:
- Explainability: AI systems must be transparent enough for clinicians to understand how they make decisions.
- Bias and Fairness: the FDA scrutinizes the data used to train AI models to ensure that models are not biased toward certain populations.
- Adaptiveness: AI technologies that continuously learn (adaptive AI) are under special scrutiny, and developers must prove that their learning processes will not compromise patient safety.
- Data privacy compliance: HIPAA, GDPR, and so on. Most commonly used tools like Open AI, however, are often not inherently compliant and it’s not clear right now how to build a completely compliant AI system, at the level of the model, even if it is aware of the compliance rules — they can be breached with clever prompt engineering.
So, as said above most startups concentrate on things that do not require FDA approval and have the minimal risk profile.

What are the areas in which AI can have the most impact?
Accelerating Drug Discovery: AI has the potential to significantly reduce drug discovery timelines, saving a lot of resources and enabling faster delivery of life-saving medications to patients. Good examples are AlphaFold and AlphaProteo.
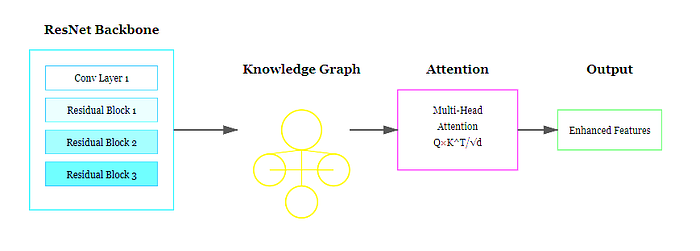
Advancing Medical Imaging: generating synthetic medical images for training AI models, augmenting real images to improve quality, and improving automated anomaly detection.
Revolutionizing Personalized Medicine: AI can analyze extensive patient data to tailor treatment and predict individual responses to therapies, pushing the boundaries of personalized care. AI can analyze genomic data to pinpoint genetic mutations and variations linked to disease. By leveraging a patient’s genetic profile, healthcare providers can design targeted therapies that are more effective and result in fewer side effects. For example, AI algorithms are being used to interpret genomic data for cancer patients, helping oncologists select the most suitable chemotherapy or immunotherapy based on the unique genetic features of the patient’s tumor.
Enhancing Medical Training: AI-generated simulations of diseases and medical procedures provide healthcare professionals with a safer, more effective platform to refine their skills without relying on real-world cases.
Optimizing Telemedicine and Virtual Care: AI-powered chatbots can answer basic medical queries and triage patients, easing the burden on healthcare workers while expanding access to timely medical advice.
Wellness and Preventive Care: AI-driven platforms that analyze user data (e.g., wearables, mobile apps) to provide personalized wellness recommendations, nutrition advice, or activity tracking.
Mental Health and Well-being Solutions: tools that help users track mental health (e.g., mood tracking, stress management) or offer personalized mental wellness programs.
AI for Administrative and Operational Efficiency: AI systems that streamline healthcare operations (e.g., reducing patient wait times, optimizing appointment scheduling, improving supply chain logistics).
Augmenting providers to remove a lot of routine tasks and allows providers to concentrate on the patients. I would like to concentrate on the last one a bit more. Healthcare is about human connection and communication a lot more than anything, and now we have lost a bit of that and now it is about gathering information and protocols. Now, AI is a technology that will allow providers to concentrate on patients by automating note-taking, preparation for the meeting, and research after the meeting
Also, it is important to point out that AI is multimodal (video, images, text, sound, subdivided to chemistry or like Alphafold — protein folding and so on), so there are a lot of synergies if we connect multiple silos of data that healthcare institutions have. AI allows to connect dots that humans can’t, because of the scale. So AI can actually work on the intersection of different areas.
On the integration side, aside from regulation hurdles, there are natural forces that slow down progress. Existing workflows in health systems are not like tech systems (say a cloud computing system). They are very hard to change, and oftentimes it is easier to integrate a less advanced or even outdated solution if it fits the system well rather than the most advanced solution.
The adoption of different Electronic Health Record (EHR) systems and other technological tools further adds to the complexity and variability of clinical workflows. When healthcare providers and institutions use disparate systems that do not communicate seamlessly, it can lead to fragmented data, redundant testing, and delays in care. The lack of interoperability between systems exacerbates workflow inefficiencies and variability. This is a part that tech people often do not understand. Tech changes fast, people change very slowly. Oftentimes the adoption is limited by trust so AI solutions are deployed with the speed of trust.
Validating and measuring success
Generative AI and predictive models require distinct testing approaches compared to structured logic systems that predict exact outcomes. With generative AI, identical inputs can yield similar yet varied results across different runs. Therefore, implementing a strong validation plan is crucial for ensuring AI accuracy. Effective testing strategies should include setting confidence thresholds (prompting the AI to either provide contextual evidence or refrain from answering), integrating human feedback in the loop, using traditional models for cross-verification (such as NLP to check contextual evidence against source material), and analyzing a confusion matrix to evaluate the rate of correct responses versus attempts. These strategies help improve model accuracy and overall performance.
Real-world cases:
Mayo Clinic, USA:
Mayo Clinic has been at the forefront of integrating AI into healthcare, particularly in radiology and cardiology. AI algorithms have been developed to assist in the interpretation of medical images, such as detecting early signs of heart disease from echocardiograms or analyzing MRI and CT scans to identify tumors. For example, the clinic has partnered with companies like Google and Nference to build machine-learning models that can predict outcomes and personalize treatments for patients with conditions like heart disease, cancer, and liver disease.
Zebra Medical Vision, Israel:
Zebra Medical Vision, an AI-based imaging analytics company, provides healthcare systems around the world with AI tools to analyze radiological images. Their AI models are used to detect a wide range of conditions, including cardiovascular diseases, lung disease, liver disease, and bone fractures. The system has been implemented in multiple hospitals, helping radiologists quickly and accurately diagnose conditions by reviewing large volumes of images at a fraction of the time it would take manually.
John Radcliffe Hospital, UK:
John Radcliffe Hospital in Oxford has developed a collaboration with the University of Oxford and Google DeepMind to use AI in the detection of acute kidney injury (AKI). The system analyzes patients’ blood test results and other health data to predict the onset of AKI up to 48 hours in advance. Early detection of AKI can significantly reduce patient mortality rates, as it allows clinicians to intervene sooner and prevent further kidney damage.
Chang Gung Memorial Hospital, Taiwan:
Chang Gung Memorial Hospital has implemented AI to improve precision medicine in the treatment of liver diseases, which are particularly prevalent in Taiwan. The hospital’s AI system analyzes genetic information and medical histories to predict which patients are most likely to benefit from certain treatments. This AI-powered approach helps physicians make more accurate treatment decisions, leading to better outcomes for liver cancer patients and those with chronic liver diseases.
Apollo Hospitals, India:
Apollo Hospitals has partnered with Microsoft to develop an AI-based system for predicting cardiovascular diseases. The system analyzes patient data, including medical history and lifestyle factors, to predict the risk of heart disease. This AI tool is particularly important in India, where heart disease is a leading cause of death. The system helps healthcare providers identify high-risk individuals early, enabling them to take preventive measures and reduce the likelihood of adverse cardiovascular events.
Karolinska University Hospital, Sweden:
Karolinska University Hospital has implemented AI to streamline the process of diagnosing and treating brain tumors. Using AI-powered imaging tools, the hospital’s medical teams can more quickly identify brain tumors and plan treatment strategies. This has led to more precise and timely interventions, improving patient outcomes. Additionally, Karolinska uses AI in drug discovery research, accelerating the development of new therapies for a range of diseases.
Mount Sinai Health System, USA:
Mount Sinai has integrated AI into its clinical workflows, particularly in the areas of imaging and disease prediction. For example, Mount Sinai uses deep learning algorithms to analyze chest X-rays and predict the likelihood of various diseases, including pneumonia and COVID-19. The system provides fast, accurate diagnostics that help doctors make better-informed decisions. In addition, Mount Sinai has used AI to predict patient outcomes for diseases like sepsis and heart failure, allowing clinicians to intervene early and improve patient care
Beth Israel Deaconess Medical Center (BIDMC), USA:
BIDMC has integrated AI algorithms into their clinical workflows, particularly in critical care settings, to predict patient deterioration. These predictive models use data from various monitoring devices and electronic health records to identify early warning signs of potential complications, allowing healthcare teams to intervene sooner. While BIDMC utilizes AI to enhance clinical decision-making, the “eICU” refers to a broader telemedicine program rather than a specific AI-driven system. However, the use of machine learning and predictive analytics at BIDMC has contributed to improved patient outcomes by reducing mortality rates and shortening hospital stays.
Moorfields Eye Hospital, UK:
In collaboration with Google DeepMind, Moorfields Eye Hospital has implemented AI technology to analyze retinal scans. This AI system, trained on thousands of retinal images, can detect over 50 different eye conditions with a level of accuracy comparable to leading ophthalmologists. By significantly speeding up the diagnosis process, this technology enables earlier detection and treatment of eye diseases, helping to prevent vision loss in many patients.
Memorial Sloan Kettering Cancer Center (MSKCC), USA:
Memorial Sloan Kettering Cancer Center (MSKCC) collaborated with IBM Watson for Oncology to support personalized cancer treatment decisions. Watson for Oncology analyzes patient data and cross-references the latest medical research to recommend evidence-based treatment options. However, despite its initial promise, the system faced challenges in clinical practice, and its effectiveness has been called into question. While it has contributed to advancing the use of AI in oncology, MSKCC has since reduced its reliance on Watson for Oncology due to concerns about the accuracy and practical utility of its recommendations.
Conclusions
AI is a very promising tool in healthcare and over the years is going to change the industry tremendously. Right now AI applications are limited and still in the exploration phase, so we have a long way to go.
Join thousands of data leaders on the AI newsletter. Join over 80,000 subscribers and keep up to date with the latest developments in AI. From research to projects and ideas. If you are building an AI startup, an AI-related product, or a service, we invite you to consider becoming a sponsor.
Published via Towards AI
Take our 90+ lesson From Beginner to Advanced LLM Developer Certification: From choosing a project to deploying a working product this is the most comprehensive and practical LLM course out there!
Towards AI has published Building LLMs for Production—our 470+ page guide to mastering LLMs with practical projects and expert insights!
Discover Your Dream AI Career at Towards AI Jobs
Towards AI has built a jobs board tailored specifically to Machine Learning and Data Science Jobs and Skills. Our software searches for live AI jobs each hour, labels and categorises them and makes them easily searchable. Explore over 40,000 live jobs today with Towards AI Jobs!
Note: Content contains the views of the contributing authors and not Towards AI.